An Actionable Framework for Health Care and Public Health Collaboration:
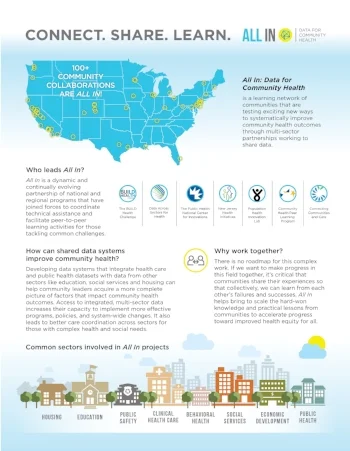
Health professionals working to protect and improve health in communities and across the nation realize that none of our distinct systems – not health care, public health, nor social services – is fully equipped to accomplish its mission alone. There is mounting recognition that to truly improve health outcomes in the U.S. and curb chronic diseases there must be an interdisciplinary, coordinated, and cross-sector approach to address acute conditions and the upstream social factors that contribute to poor health outcomes. This approach requires transformation of the way the health and human service systems traditionally interact.
In pursuit of this goal, members of the PUBLIC HEALTH LEADERSHIP FORUM (PHLF) and HEALTH CARE TRANSFORMATION TASK FORCE (HCTTF) developed a framework to help catalyze and facilitate collaborative working relationships between the public health and health care sectors. Such partnerships are an essential component of the “comprehensive community wellness approach,” one in which effective, collaborative relationships across sectors ensure more seamless care and prevention services for all. Under this approach, public health, health care, and social service and community organizations intentionally build high-functioning partnerships to address health needs in their communities, and invest in the time, staff, information platforms, and oversight structures needed to sustain them. The framework outlines essential elements of collaboration and presents key tactics and strategies for forming or reshaping effective partnerships.
Public Health Leadership Forum | June 13, 2018
This piece appears in Health Care Transformation’ Task Force’s Transformation Resources Page.
Read More